COVID-19: The impacts
PLEASE NOTE: (4th April 2022)
The availability of COVID-19 data is changing and we are still not totally sure how data will be provided to us and how in turn we can present the data to you. Please check back here for any updates as we are informed.
The impacts of Coronavirus (COVID-19)
How can this information help?
To help us and you understand more about the virus, its impact and the future then we have collated, and will continue to, a range of data sources, literature and information that helps us all to respond in the most appropriate way possible.
We will endeavour to keep the information up to date and adding new and relevant content. If you are aware of additional information or feel we could develop the page then please get in touch phintelligence@wirral.gov.uk
COVID-19 Data COVID-19 Response
Early research
Public Health England (PHE) published a COVID-19: review of disparities in risks and outcomes (rapid review) into how different factors have affected COVID-19 risk and outcomes. This research work confirmed that COVID-19 has replicated existing health inequalities and in some cases exacerbated them.
The effects of the pandemic
Men and Women
Nationally
- More women have contracted coronavirus than men
Source: Disparities in the risk and outcomes of COVID-19
Wirral
- See COVID-19 data page where more information may be available
Older People
Risk for severe illness increases with age
As you get older, your risk for severe illness from COVID-19 increases. For example, people in their 50s are at higher risk for severe illness than people in their 40s.
Similarly, people in their 60s or 70s are, in general, at higher risk for severe illness than people in their 50s.
The greatest risk for severe illness from COVID-19 is among those aged 85 or older.
Wirral
- See COVID-19 Data page for more information
Further Evidence
Mortality among Care Home Residents in England during the first and second waves of the COVID-19 pandemic: an analysis of 4.3 million adults over the age of 65
-
In this research it suggests that the first COVID-19 wave had a disproportionate impact on care home residents in England compared to older private home residents.
-
A degree of immunity, improved protective measures or changes in the underlying frailty of the populations may explain
the lack of an increase in the relative mortality risks during the second wave.
-
The care home population should be prioritised for measures aimed at controlling the spread of COVID-19.
Is older age associated with COVID-19 mortality in the absence of other risk factors?
-
Older people have been reported to be at higher risk of COVID-19 mortality.
-
This general population cohort study of 470,034 participants study explored the factors mediating this association and whether older age was associated with increased mortality risk in the absence of other risk factors.
-
Overall, participants aged ≥75 years were at 13-fold (95% CI 9.13-17.85) mortality risk compared with those <65 years.
-
Participants aged ≥75 without additional risk factors were at 4-fold risk (95% CI 1.57-9.96, P = 0.004) compared with all participants aged <65 years.
-
Higher COVID-19 mortality among older adults was partially explained by other risk factors. 'Healthy' older adults were at much lower risk.
-
Nonetheless, older age was an independent risk factor for COVID-19 mortality.
The experience of older people instructed to shield or self-isolate during the Covid-19 pandemic
-
A vital weapon in the fight against Covid-19 has been the shielding of clinically extremely vulnerable individuals at high risk, and instructions to clinically vulnerable people at moderate risk to stay at home and avoid face-to-face contact as far as possible.
-
The consequences of this advice for mental health and wellbeing are not well understood.
-
The English Longitudinal Study of Ageing (ELSA) Covid-19 Substudy provided an opportunity to evaluate the impact on mental health, quality of life, social connectedness, worries, and health-related behaviour in more than 5,800 older men and women (mean age 70 years)
The experience of older people with multimorbidity during the Covid-19 pandemic
-
The risk of severe Covid-19 disease is known to be higher in older individuals with multiple longterm health conditions (multimorbidity).
-
This ELSA briefing reports on the latest findings from the English Longitudinal Study of Ageing Covid-19 Substudy (ELSO) on the experiences of older people with multimorbidity during the pandemic.
Poorer areas
PHE and National Institute for Health Research (NIHR) found that:
-
The mortality rates from COVID-19 in the most deprived areas have been more than double the least deprived areas, for both males and females.
-
This is greater than the ratio for all cause mortality between 2014 to 2018 indicating greater inequality in death rates from COVID-19 than all causes.
-
Survival among confirmed cases, after adjusting for sex, age group, ethnicity and region was lower in the most deprived areas, particularly among those of working age where the risk of death was almost double the least deprived areas.
-
People in deprived areas are more likely to be diagnosed and to have poor outcomes following diagnosis than those in less deprived areas.
Source: Disparities in the risk and outcomes of COVID-19
Wirral
- See COVID-19 Data page where more information may be available
National
Covid-19 and the Northern Powerhouse Tackling inequalities for UK health and productivity.
-
The Northern Health Science Alliance commissioned this report to understand the impact of the COVID-19 pandemic on health and productivity in the Northern Powerhouse
-
Also to explore the opportunities for ‘levelling up’ regional health and productivity, across the life course.
-
The report shows the unequal health and economic impacts of COVID-19 on the Northern Powerhouse.
-
As it develops its post-COVID-19 ‘levelling up’ industrial strategy, central government should pay particular attention to the importance of supporting the physical and mental health and development of the Northern Powerhouse as a route to increased prosperity.
Living in poverty was bad for your health before COVID-19
-
This long read looks at the link between health and income.
-
It explores the nature of the economic shocks experienced in recent years, including those stemming from COVID-19, and the consequences these might have on people’s health.
-
It then considers how we might use the current crisis to build a fairer and healthier society.
Black, Asian and minority ethnic population
PHE and National Institute for Health Research (NIHR) found that:
-
BAME groups are more likely to be tested and to test positive
-
BAME groups have increased risk of death associated with Covid-19
-
Ethnicity and income inequality are independently associated with Covid-19 mortality
-
BAME group population are more likely to:
-
live in overcrowded housing
-
work in occupations which palce them at increased exposure to Covid-19
-
Use public transport to travel to work
-
-
BAME group population are less likely to:
-
seek care when needed
-
speak up when they have concerns about PPE or testing
-
Source: Beyond the data: Understanding the impact of COVID-19 on BAME groups
Wirral
-
See COVID-19 Data page where more information may be available
Further Evidence
Ethnic inequalities in Covid-19 mortality: a consequence of persistent racism
-
This briefing (published in collaboration between Runnymede Trust and the Centre of Dynamics of Ethnicity) discusses the reasons for ethnic minority people experiencing a much higher risk of Covid-19-related death.
-
Ethnic inequalities, in relation to Covid-19, mirror longstanding ethnic inequalities in health.
-
A large body of evidence has shown that these inequalities are driven by social and economic inequalities, many of which are the result of racial discrimination.
Unequal impact? Coronavirus and BAME people (December 2020)
-
This Women and Equalities Committee report outlines the findings of an inquiry that aimed to explore the pre-existing inequalities facing people from ethnic minorities and how these inequalities have impacted on their vulnerability to the virus.
-
It makes a series of recommendations to help mitigate the impacts of the pandemic on ethnic minority groups
Ethnic inequalities in Covid-19 are playing out again – how can we stop them?
-
Despite the inequalities exposed earlier this year, there has been little effort to stop Covid-19 hitting minority ethnic communities hardest as we enter the second wave. Without urgent action, the effects of pandemic are set to be felt unequally again.
-
IPPR and Runnymede Trust estimate over 58,000 and 35,000 additional deaths from Covid-19 would have occurred if the white population had experienced the same risk of death from Covid19 as the black and south Asian populations respectively.
-
IPPR estimate comorbidities lead to the black population being only five per cent more likely to die from Covid-19 than the white population.
-
Higher deprivation levels explain the disparities to a greater extent, but the majority of the additional risk of death from Covid-19 experienced by minority ethnic communities is unexplained
Updating ethnic contrasts in deaths involving the coronavirus (Covid-19), England and Wales : deaths occurring 2 March to 28 July 2020
-
This ONS report confirms that when adjusting for age, rates of death involving Covid-19 remain greater for most ethnic minority groups, and most notably so for people of black African, black Caribbean, Bangladeshi and Pakistani ethnic backgrounds.
-
The statistical modelling shows that a large proportion of the difference in the risk of Covid-19 mortality between ethnic groups can be explained by demographic, geographical and socio-economic factors.
-
It also found that although specific pre-existing conditions place people at greater risk of Covid-19 mortality generally, this does not explain the remaining ethnic background differences in mortality
How coronavirus has affected equality and human rights
-
This Equality and Human Rights Commission report summarises evidence that helps in understanding the effects of the coronavirus (Covid-19) pandemic on different groups in society.
-
It highlights potential long-term risks to equality and human rights covering key issues in the areas of work; poverty; education; social care; and justice and personal security.
-
It makes targeted recommendations for the UK, Scottish and Welsh governments to ensure equality and human rights considerations are integrated into the policy response to the pandemic.
Quarterly report on progress to address Covid-19 health inequalities (October 2020)
- This Race Disparities Unit report summarises the work undertaken by the Minister for Equalities and government departments on Covid-19 disparities.
Black, Asian and minority ethnic groups at greater risk of problem debt since Covid-19
-
Before Covid-19, around 4 per cent of households in the UK were identified as having ‘problem debt’; that is, debt which represents a high proportion of disposable income, includes arrears on household bills or credit commitments, and feels like a heavy burden to the people who owe the money.
-
Before Covid-19, ethnic minority groups were more likely to say that they were ‘struggling financially’, and to live in a household which was behind on bills or housing payments. 7% of people across the population reported that they were struggling financially, but for people from non-white groups the figure was between 12 and 18 per cent.
-
Across the population, around 5% of those employed in January/February were no longer working in June.
-
Amongst ethnic minority groups, the equivalent figure was 13%. As such, they were nearly three times as likely to have moved from employment to not working.
-
People from black, Asian and minority ethnic groups are also likely to be particularly vulnerable because they are more likely to rent than to own their home.
-
Rates of renting are substantially higher for these groups than for the population as a whole.
Over-exposed and under-protected: the devastating impact of COVID-19 on black and minority ethnic communities in Great Britain
-
This report illuminates why BAME groups are at greater risk from COVID-19:
-
they are more likely to be working outside their home,
-
more likely to be using public transport,
-
more likely to be working in key worker roles,
-
less likely to be protected with PPE and
-
more likely to live in multigenerational, overcrowded housing, so much less able to self-isolate and shield
-
Understanding the impact of COVID-19 on Black Asian Minority Ethnic (BAME) communities.
-
PHE (June 2020) published a rapid review into how different factors have affected COVID-19 risk and outcomes.
-
This work confirmed that COVID-19 has replicated existing health inequalities and in some cases exacerbated them.
-
In relation to Black, Asian Minority Ethnic (BAME) communities, then specific work was undertaken to learn more about factors that may be influencing the impact of COVID-19.
-
PHE has published a summary of this work, which includes recommendations based upon stakeholder’s requests for action for strategies addressing inequalities.
-
These insights will form the basis of the next steps being taken forward by the Equalities Minister.
Beyond the data: Understanding the impact of COVID-19 on BAME groups (June 2020)
-
There is clear evidence that COVID-19 does not affect all population groups equally.
-
Many analyses have shown that older age, ethnicity, male sex and geographical area, for example, are associated with the risk of getting the infection, experiencing more severe symptoms and higher rates of death.
-
This work was commissioned by the Chief Medical Officer for England to understand the extent that ethnicity impacts upon risk and outcomes.
COVID-19 and Black, Asian and minority ethnic communities (House of Commons Library briefing) (17 June 2020).
-
This pack has been prepared ahead of the debate to be held in the Commons Chamber on Thursday 18 June 2020 on the effect of COVID-19 on Black, Asian and Minority Ethnic (BAME) communities.
House of Commons Library Briefing: Sources of statistics on inequalities between ethnic groups (June 2020)
-
This briefing paper provides a list of links to statistical and other related resources on differences by ethnic group in a range of topics including health, justice, employment and income.
-
Material is listed by type of resource (e.g. House of Commons Library publications, government publications and independent reviews).
The impact of COVID-19 on BME communities and health and care staff
-
This NHS Confederation briefing considers the evidence on the impact of COVID-19 on black and minority ethnic (BME) communities and health and care staff.
-
It explores potential underlying factors, recommends areas for improvement and offers practical advice on how to mitigate risks.
-
Intended for senior health and care leaders, it aims to inform decision making and influence change.
Are some ethnic groups more vulnerable to COVID-19 than others?
- This Institute for Fiscal Studies report brings together evidence on the unequal health and economic impacts of COVID-19 on the UK’s minority ethnic groups, presenting information on risk factors for each of the largest minority groups in England and Wales.
Inequalities in COVID-19 mortality related to ethnicity and socioeconomic deprivation (May 2020)
-
This study from the University of Liverpool reports analysis of people across 147 local authorities to see whether those with higher proportion of people from BAME groups and levels of deprivation were also likely to have higher numbers of covid-related deaths.
-
Both ethnicity and income deprivation were independently associated with mortality and these associations were independent of each other, and remained after controlling for population density, the duration of the epidemic and the proportion of older residents.
Coronavirus (COVID-19) related deaths by ethnic group, England and Wales: 2 March 2020 to 10 April 2020, Office of National Statistics, 7th May 2020
-
This ONS study used ethnicity data from the 2011 census alongside death certificate registration to 10th April 2020.
-
This provisional analysis reported that the risk of death involving the coronavirus (COVID-19) among some ethnic groups was significantly higher than that of those of White ethnicity.
Emerging findings on the impact of COVID-19 on black and minority ethnic people, 20th May 2020
-
The Health Foundation put together a chart series to review the evidence that black and minority ethnic communities are at greater risk of catching and dying from the virus.
-
It also considers the reasons why these groups might be at greater risk using evidence from the Office of National Statistics Labour Force survey.
BAME COVID-19 DEATHS – What do we know? Rapid data & evidence review, May 2020
-
The rapid data and evidence synthesis completed in four days and published on the Centre for Evidence-based medicine website.
-
It reviewed evidence identified through a Google Scholar literature search and identified additional studies by screening references of included studies and through searching of websites of different government, multinational agencies and COVID-19 resource aggregators.
Jobs and occupations
National
-
A total of 10,841 COVID-19 cases were identified in nurses, midwives and nursing associates registered with the Nursing and Midwifery Council. Among those who are registered, this represents 4% of Asian ethnic groups, 3.1% of Other ethnic groups, 1.7% of White ethnic groups and 1.5% of both Black and Mixed ethnic groups. This analysis did not look at the possible reasons behind these differences, which may be driven by factors like geography or nature of individuals’ roles.
-
ONS reported that men working as security guards, taxi drivers and chauffeurs, bus and coach drivers, chefs, sales and retail assistants, lower skilled workers in construction and processing plants, and men and women working in social care had significantly high rates of death from COVID-19.
-
PHE analysis expands on this and shows that nursing auxiliaries and assistants have seen an increase in all cause deaths since 2014 to 2018.
-
For many occupations, however, the number of deaths is too small to draw meaningful conclusions and further analysis will be required.
Source: Disparities in the risk and outcomes of COVID-19
Wirral
-
See COVID-19 Data page where more information may be available
Further Evidence
Characteristics of people testing positive for the coronavirus (COVID-19) in England from the COVID-19 Infection Survey
Main points
-
In this ONS article, they refer to the number of coronavirus (COVID-19) infections within the community population in England; community in this instance refers to private residential households, and it excludes those in hospitals, care homes or other institutional settings.
-
Infections refer to those identified from a positive test for coronavirus (COVID-19) from a swab taken from someone’s nose and throat; this means there was evidence that they had the coronavirus when the swab was taken.
-
Individuals working outside the home show higher rates of positive swab tests than those who work from home.
-
Over the study period, infection rates are higher for those working in patient-facing healthcare or resident-facing social care roles than for people not working in these roles.
Care Home residents and staff
National
-
Data from the Office for National Statistics (ONS) shows that deaths in care homes accounted for 27% of deaths from COVID-19 up to 8 May 2020.
-
The number of deaths in care homes peaked later than those in hospital, in week ending 24 April.
Source: Disparities in the risk and outcomes of COVID-19
Wirral
-
See COVID-19 Data page where more information may be available
People with multiple illnesses
Risk for severe illness increases with multiple conditions
As you get older, your risk for severe illness from COVID-19 increases and this is closely linked to co-morbidities that include:
-
Chronic kidney disease
-
COPD (chronic obstructive pulmonary disease)
-
Immunocompromised state (weakened immune system) from solid organ transplant
-
Obesity (body mass index [BMI] of 30 or higher)
-
Serious heart conditions, such as heart failure, coronary artery disease, or cardiomyopathies
-
Sickle cell disease
-
Type 2 diabetes mellitus
Wirral
-
See COVID-19 Data page where more information may be available
Further Evidence
Deaths of people identified as having learning disabilities with Covid-19 in England in the spring of 2020 (November 2020)
-
This review, commissioned by the Department of Health and Social Care, looked at: deaths from Covid-19 of people with learning disabilities; factors impacting the risk of death from Covid-19 of people with learning disabilities; and deaths in care settings of people with learning disabilities.
-
It found the death rate up to six times higher from coronavirus during the first wave of the pandemic than the rate in the general population.
Learning Disability (House of Commons Library) (June 2020)
-
House of Commons Library briefing on policies and services for people with a learning disability in England. Section 1 provides a summary of the impact of coronavirus on people with learning disabilities in England.
-
The briefing also looks at recent policy changes in the areas of employment, welfare and education.
Local Evidence
-
Rapid evaluation of targeted work to increase COVID-19 vaccination uptake in Wirral (August 2022)
The roll out of the Covid-19 vaccine programme has been a breakthrough and minimised the health, social and economic impact of the pandemic achieved through high levels of vaccination. Differences in health outcomes, between groups and communities, is an enduring challenge. To minimise these differences in the Covid-19 vaccine programme the Covid-19 Vaccination Health Inequalities Group was set up in April 2021 to drive forward a range of targeted interventions to address this variation. The interventions were informed by epidemiology, surveillance data, evidence and localintelligence and the methods used were outreach delivery, communication and engagement and direct follow up. The purpose of this evaluation report is to present the outcomes of subsequent interventions, delivered between November 2021 and August 2022, that continued to address the differences in vaccine uptake.
-
Risk & Outcomes of COVID-19 in Wirral (December 2021)
This is a descriptive review of data on disparities in the risk and outcomes from COVID-19 in Wirral between 01/03/2020 to 30/06/2021 (first 18 months of the pandemic). It updates a previous version of this report which examined the first period of the pandemic in Wirral and covered 01/03/2020 to 30/06/2020 (first 3 months of the pandemic). -
COVID-19 Mortality in Wirral (March 2021)
This is a descriptive review of data on mortality from COVID-19 in Wirral during 2020. The review presents findings based on surveillance data available Wirral Intelligence Service at the time of publication, including that available through linkage to other health data sets (e.g., via the Wirral Care Record). -
Risk & Outcomes of COVID-19 in Wirral (August 2020)
This was a descriptive review of data on disparities in the risk and outcomes from COVID-19 in Wirral between March and June 2020. The review presents findings based on surveillance data available Wirral Intelligence Service at the time of publication, including that available through linkage to other health data sets (e.g. via the Wirral Care Record). The format is based on the Public Health England report, “Disparities in the risk and outcomes of COVID-19” published in June 2020 and takes a population health approach.
What are the impacts?
A rapid evidence review produced by Public Health Institute for Cheshire and Merseyside Public Health collaborative service (CHAMPS) suggests the impacts of COVID-19 have not been felt equally – the pandemic has both exposed and exacerbated longstanding inequalities in society.
As we move from the response phase into recovery, the direct and wider impacts of the pandemic on individuals, households and communities will influence their capacity to recover.
A further resource is the wider impacts of COVID-19 on health monitoring tool. This is a national monitoring tool that brings together metrics to assess the wider impacts of COVID-19. Another resource is the Institute of Fiscal Studies report (February 2021)that examines the impact of the pandemic on educational, economic, social and health inequalities in the UK. It outlines data and evidence on the groups that have been most heavily impacted by widening inequalities and COVID-19.
Social Factors
Impacts on family, friends and communities
The COVID-19 pandemic has had both positive and negative impacts on social and community networks. There is evidence of increased civic participation in response to the pandemic and a positive impact on social cohesion. Thousands of new volunteer groups have been established in communities across the country and the majority of adults believe the country will be more united and kinder following the pandemic.
However, social isolation and loneliness have impacted on wellbeing for many. There are also serious concerns about how the combination of greater stress and reduced access to services for vulnerable children and their families may increase the risk of family violence and abuse. Compounding this, safeguarding issues have been largely hidden from view during lockdown.
Further evidence
Loneliness, social isolation, and COVID-19
-
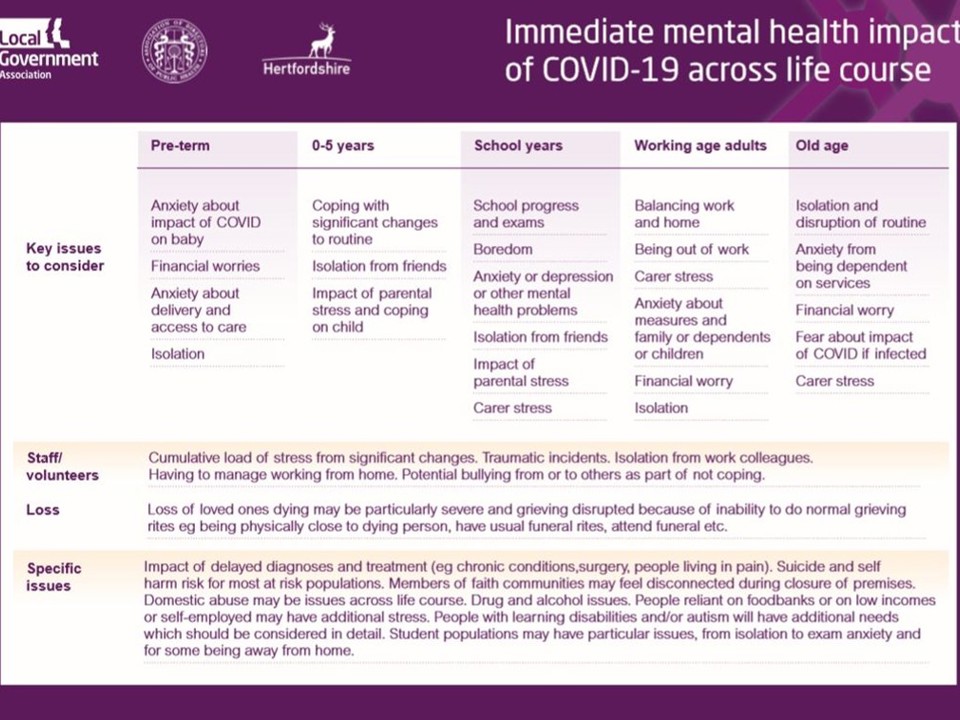
The Local Government Association (LGA) and Association of Directors of Public Health (ADPH) have jointly produced this practical advice for Directors of Public Health and others leading the local response to the loneliness and social isolation issues arising from the COVID-19 outbreak.
-
It follows on from our guidance about the public mental health impacts across the life course.
How has COVID-19 and associated lockdown measures affected loneliness in the UK?
-
This What Works Centre for Wellbeing briefing highlights findings from the Covid Social Study, as part of ongoing data analysis work with University College London.
-
This study has surveyed more than 70,000 people since March 2020, asking different questions about their experiences and wellbeing over the past few months, including asking people about loneliness.
Volunteering during the COVID-19 pandemic: What are the potential benefits to people’s well-being? (April 2020)
Coronavirus and loneliness, Great Britain: 3 April to 3 May 2020
- The Office for National Statistics has published an analysis of loneliness in Great Britain during the coronavirus (COVID-19) pandemic from the Opinions and Lifestyle Survey.
Misinformation in the COVID-19 infodemic
-
This House of Commons Digital, Culture, Media and Sport Committee report finds that online misinformation about COVID-19 was allowed to spread virulently across social media without the protections offered by legislation promised by the government in the Online Harms White Paper published in April 2019.
-
The report details evidence on a range of harms from dangerous hoax treatments to conspiracy theories that led to attacks on 5G.
The psychology of loneliness: why it matters and what we can do
This Campaign to End Loneliness report looks at how psychological approaches can help tackle loneliness.
-
It is focused on older people but has lessons for all adults. It gathers the current research and evidence available to us about what we can learn from psychology, as well as making policy recommendations for how this learning can be applied and help the millions of lonely people across the UK. engineers.
-
The Committee calls for the government to make a final decision on the appointment of an independent online harms regulator immediately.
Coronavirus and the social impacts on the countries and regions of Britain: Office for National Statistics - April 2020
Economic Factors
Impact on money and resources
The economic impact of the social distancing and lockdown measures has seen an increase in people signing up for Universal Credit and Jobseeker’s Allowance benefits. Young workers and low earners have been impacted the most and household incomes have fallen particularly among the lowest earners. The predicted economic downturn will have significant health impacts in the short and longer term.
Impact on education and skills
There are various strands of emerging evidence to suggest that children and young people may be hit hardest by the social distancing and lockdown measures. School closures risk exacerbating existing inequalities in educational attainment. Surveys suggest that the richest
households are more likely to be offered active help from school, and that they are spending more hours a day on home learning.
Further Evidence
Pandemic pressures
-
This Resolution Foundation note explores why so many low-income families report spending more, not less, since Covid-19 gripped the nation in spring 2020.
-
It brings together the findings from two online surveys of a representative sample of working-age adults in the UK fielded by the Resolution Foundation in May and September 2020, and a number of vivid accounts from parents and carers themselves, drawn from the ongoing Covid Realities participatory research programme.
-
The report highlights how increased financial worries amplify the negative impact of the pandemic on the mental health of parents and carers on a low income.
UK poverty 2020/21
-
This Joseph Rowntree Foundation report highlights early indications of how poverty has changed in our society since the start of the coronavirus outbreak, as well as the situation revealed by the latest poverty data, collected before the outbreak.
-
It examines overall changes to poverty, with sections looking at the impact of work, the social security system and housing.
-
It also benefits from powerful insights from members of JRF's Grassroots Poverty Action Group, who have direct experience of living on a low income.
Covid-19 and the Northern Powerhouse: tackling inequalities for UK health and productivity
-
According to this report the Northern Health Science Alliance, the north of England’s economy has been hit harder than the rest of the country's during the Covid-19 pandemic.
-
It estimates the economic cost of the increased mortality in the north during the pandemic at £6.86 billion, and the reductions in mental health in the region due to the pandemic could cost the UK economy up to £5 billion in reduced productivity. (Report)
Living in poverty was bad for your health before COVID-19
-
This long read looks at the link between health and income.
-
It explores the nature of the economic shocks experienced in recent years, including those stemming from COVID-19, and the consequences these might have on people’s health.
-
It then considers how we might use the current crisis to build a fairer and healthier society.
Lockdown, lifelines and the long haul ahead: the impact of Covid-19 on food banks in the Trussell Trust network
- This report presents findings of research carried out by the Trussell Trust and Heriot Watt University.
- It estimates that 846,000 food parcels will need to be provided to people in crisis during October to December 2020 – a 61 per cent increase on last year.
- It also estimates that an additional 670,000 people will be destitute by the end of the year, meaning they cannot afford essentials such as housing, energy and food.
Poverty in the pandemic: The impact of coronavirus on low-income families and children (August 2020)
Coronavirus has left low-income families struggling with a significant deterioration in living standards and high stress levels a new report from Child Poverty Action Group and the Church of England finds.
-
Families who responded in July and early August were even less optimistic about their financial situation than those who responded in May or June.
Some key findings from the report include:
-
8 in 10 hard-up families said they were financially worse off as a result of the pandemic
-
Almost half have had physical or mental health problems because of coronavirus
-
9 in 10 survey respondents said they were spending substantially more than before on food, electricity, and other essentials –usually because they have been at home much more
-
More than three-quarters of respondents said the coronavirus has affected their ability to pay for food (83%) and utilities (76%) and around half said it has affected their ability to pay for housing (47%) and child-related costs (e.g. nappies or baby products, children’s clothes – 53%).
In light of these findings, the report calls on the Government to:
-
Increase child benefit by £10 a week and add an extra £10 a week to the child element within universal credit and child tax credits
-
Extend free school meals to all families who are in receipt of universal credit or working tax credit, with a view to bringing in universal free school meals for all children in the long term
-
Abolish the benefit cap, or at least suspend it for the duration of the pandemic, to protect families whose employment has been disrupted by the crisis.
Children in lockdown: the consequences of the coronavirus crisis for children living in poverty
-
This report by the Childhood Trust documents the impact of the coronavirus (COVID-19) pandemic on disadvantaged and vulnerable children in London (though similar impacts will be felt across UK).
Coronavirus and the economic impacts on the UK: 16 July 2020
-
The indicators and analysis presented in this ONS bulletin are based on responses from the voluntary fortnightly business survey, which captures businesses’ responses on how their turnover, workforce prices, trade and business resilience have been affected.
-
These data relate to the period 15 June 2020 to 28 June 2020.
Economic impact of coronavirus: gaps in support (House of Commons Treasury Committee)
-
This unanimously agreed interim report of the inquiry into the economic impact of COVID-19 has identified key concerns relating to the following groups:
-
those newly in employment or newly self-employed;
-
those self-employed with annual trading profits in excess of £50,000;
-
directors of limited companies; and
-
freelancers or those on short-term contracts.
-
-
The report makes a series of recommendations as to how the government could effectively address these concerns.
Rainy days: an audit of household wealth and the initial effects of the coronavirus crisis on saving and spending in Great Britain
-
This Resolution Foundation report shows that those most at risk in the pandemic have the weakest private savings safety net to fall back on, while the crisis itself is exposing Britain’s wealth gaps, and the ability of low-wealth households to weather the economic storm.
COVID-19's impact on public finances and government borrowing (Nuffield Trust, July 2020)
-
This Nuffield Trust briefing highlights the immense changes to government finances in recent months precipitated by the coronavirus, and considers what this might mean for health services in future.
-
The impact of the coronavirus pandemic on public finances around the world has been immediate and massive.
-
In the UK, a combination of lockdown measures and the need for huge boosts in public spending has, in just a few months, outweighed the impact wrought by the 2008 global financial crisis.
-
In order to finance its activities, in May this year the government borrowed £55.2 billion compared to just £5.7 billion in May 2019. Increases in day-to-day borrowing – the deficit – has added to the stock of national debt, pushing it from just over 80% of GDP in May last year to nearly 101% this May.
-
This is the first time debt has exceeded total GDP since 1963.

Coronavirus and the then latest indicators for the UK economy and society (28 May 2020)
-
This ONS report uses early experimental data on the impact of the coronavirus (COVID-19) on the UK economy and society, including online price changes data.
-
These faster indicators are created using rapid response surveys, novel data sources and experimental methods.
Environmental Factors
Impact on our surroundings
People have spent far more time at home during lockdown which may play a role in exacerbating the health impacts of poor-quality housing. Further, an estimated 12% of households in England have had no access to a private or shared garden during lockdown.
Although access to public parks is more evenly distributed, inequalities exist in access to good quality and safe public green space. Air was cleaner and healthier in early lockdown, but global emissions have since rebounded to close to 2019 levels.
Impact on transport
The impact on transport has been mixed. Falls in road journeys during the early period of lockdown have generally been short-lived and there are concerns about the lasting damage that may be done to public transport systems. A positive impact has been seen with more people cycling, but it remains to be seen whether the changes to cycling infrastructure will have a lasting impact.
Impact on the food we eat
Lockdown has exacerbated food insecurity and food need; particularly among children. The number of adults who are food insecure is estimated to have quadrupled. Food banks have experienced a rapid increase in demand but alongside this have experienced reduced volunteer numbers.
Further Evidence
Accessibility and allocation of public parks and gardens in England and Wales: A COVID-19 social distancing perspective
-
This PubMed published research suggests that visiting parks and gardens supports physical and mental health.
-
They quantified access to public parks and gardens in urban areas of England and Wales, and the potential for park crowdedness during periods of high use.
-
They examined variability by city and share of flats. Around 25.4 million people (~87%) can access public parks or gardens within a ten-minute walk, while 3.8 million residents (~13%) live farther away; of these 21% are children and 13% are elderly.
-
Areas with a higher share of flats on average are closer to a park but people living in these areas visit parks that are potentially overcrowded during periods of high use.
-
Such disparity in urban areas of England and Wales becomes particularly evident during COVID-19 pandemic and lockdown when local parks, the only available out-of-home space option, hinder social distancing requirements.
-
Cities aiming to facilitate social distancing while keeping public green spaces safe might require implementing measures such as dedicated park times for different age groups or entry allocation systems that, combined with smartphone apps or drones, can monitor and manage the total number of people using the park.
Access to Health Services
Making history: health visiting during Covid-19 (September 2020)
- This collection of case studies presents a window into the working lives of health visitors and families navigating the ups and downs of the Covid-19 pandemic.
- The case studies, family stories and creative pieces contained in the report capture the pace and scale of change as health visiting services adapted to working during 'lockdown'.
Longer waits, missing patients and catching up
-
This Health Foundation analysis looks at the impact of the second wave of the Covid-19 pandemic on elective care in England.
-
The waiting list has now reached the highest level since comparable records began, with more patients experiencing long delays in diagnosis and treatment.
A telling experience: understanding the impact of Covid-19 on people who access care and support – a rapid evidence review with recommendations (October 2020)
- This Think Local Act Personal report aims to identify what worked well, and to highlight areas that people found difficult, both generally and in relation to social care during the first phase of the coronavirus pandemic, seen through the lens of personalisation
The impact of COVID-19 on community health services
-
This NHS Confederation report, produced together with NHS Providers, captures the community health sector’s response during the pandemic and showcases the achievements of community providers and their staff.
-
It seeks to learn from community providers’ experiences of the pandemic to secure much-needed transformation for the longer term, and makes a number of recommendations for support from government and the national NHS bodies to enable this.
Coronavirus: health and social care key issues and sources
-
This Commons Library briefing paper provides an overview of key issues facing the NHS and social care services during the coronavirus (COVID-19) outbreak, and links to official UK and international guidance and data.
-
It also lists other reliable sources of information in the health and social care sector, including comment from organisations representing patients, staff and service providers.
-
This briefing paper was last updated on 13 July 2020.
The hidden impact of COVID-19 on patient care in the NHS in England (July 2020)
-
This BMA report suggests that the full impact of this drastic reduction in routine NHS care in England is only now emerging.
-
Millions of patients living with health problems (including life-threatening conditions such as cancer) have been affected, with their treatment postponed or cancelled.
-
And millions of patients will have missed vital opportunities to receive initial assessment and diagnosis for health problems in the first place.
-
This is the hidden impact of the COVID-19 crisis – patient safety is being severely compromised not just by the virus itself, but by the knock-on effects of an unprecedented disruption to NHS services.
Number of people waiting over a year for treatment has increased dramatically in months since onset of pandemic (Nuffield Trust)
Chart of the Week (20th July 2020)

-
The number of people in England waiting over a year from referral by a GP to treatment has grown exponentially in the last 3 months, from 1,613 in February to 26,029 in May 2020.
-
Hospitals cancelled all routine operations around the middle of March, and specialists were diverted to work with Covid-19 patients. For patients who were already waiting for treatment, this has meant even longer waits.
-
Apart from cancer services, which have more stringent waiting targets, all specialties for which data is reported have been impacted, although year-long waits have increased most for oral surgery, ophthalmology, gynaecology, and ear, nose and throat treatments.
-
Hospitals are now re-establishing routine services, but organising services to minimise the risks of transmission in hospital mean that productivity will be affected for some time to come.
-
The number of people waiting over a year dropped dramatically from over half a million in 2007 to a few hundred in 2013.
-
As the overall waiting list has increased in the last five years, the focus has shifted towards reducing longer waits again.
-
The NHS operational plan for 2020/21 published in January 2020 had an ambition for the NHS to “stabilise and reduce waiting lists for elective care and eradicate waits of 52 weeks or more”.
-
This ambition could prove difficult to achieve in the current, and immediate future, circumstances.
More patients struggle to get through to GP practices by phone
- Results from the recent (Pre-COVID-19) GP Patient Survey found that a larger number of patients are struggling to get through to their GP via telephone.
-
However the annual exercise showed that almost all patients continue to have confidence and trust in their GP and other practice staff.
-
The survey was completed by around 740,000 patients in England ‘prior to the COVID-19 pandemic’ between January and March 2020.
-
Given changes to surgery access and COVID-19 responses to symptoms then this contact may have worsened over recent months.
Readying the NHS and adult social care in England for COVID-19
-
This report by the National Audit Office (NAO) provides a factual overview of the response by the Department of Health and Social Care (DHSC) and other bodies during March and April 2020 to prepare the NHS and adult social care in England for the COVID-19 pandemic.
Five key insights on COVID-19 and adult social care
-
The Health Foundation published two new briefings on COVID-19 and social care. Adult social care and COVID-19: Assessing the impact on social care users and staff in England so far analyses the available data on social care and gives an overview of the impact of the pandemic.
Health Behaviours
Individual health behaviours
The wider determinants of health both shape the distribution of, and trigger stress pathways associated with the adoption of unhealthy behaviours. Lockdown has impacted on these behaviours in different ways. People who were drinking alcohol the most often before lockdown are also the ones who are drinking alcohol more often and in greater quantities on a typical drinking day. People already drinking alcohol the least often have cut down in the greatest number. The impacts on smoking appear to be more positive, with smokers showing an increased motivation to quit and to stay smoke free during the pandemic.
Findings are less clear in relation to diet. Non-UK studies show decreased physical activity and increased eating and snacking during lockdown. In England, physical activity behaviours among children and adults have been disrupted by lockdown. Although some groups have continued to be physically active, groups that were least active before lockdown are finding it harder.
Further Evidence
Alcohol consumption and harm during the COVID-19 pandemic
-
A report collating data on alcohol consumption and alcohol-related harm in England during the COVID-19 pandemic and comparing it to data from previous years.
-
Alcoholic liver deaths increased by 21% during year of the pandemic.
-
Increased alcohol consumption during the pandemic, particularly amongst heavy drinkers, is likely driving an unprecedented acceleration in alcoholic liver disease deaths.
Smoking and COVID-19
-
Smokers are generally at greater risk of respiratory viruses. Smoking damages the lungs and airways and weakens the immune system, making it harder to fight infection.
-
The hand to mouth action of smoking provides another potential route of entry into the body for viruses. Smokers are more likely than non-smokers to have pre-existing conditions such as respiratory disease, cardiovascular disease and type 2 diabetes which are associated with poorer outcomes for COVID-19.
-
Analysis of data from 2.4 million UK users of the COVID Symptom Tracker app indicated that current smokers were 14% more likely than non-smokers to develop the three "classic" symptoms – fever, persistent cough and shortness of breath; and current smokers who tested positive for COVID-19 were more than twice as likely as non-smokers to be hospitalised.
-
The international evidence on COVID-19 outcomes for smokers is mixed and developing. A living rapid evidence review by researchers at the Royal Veterinary College and University College London finds uncertainty regarding the relationship between smoking status and SARS-CoV-2 infection, hospitalisation, disease severity and mortality from COVID-19 disease.
-
According to the latest version of the review, recorded smoking prevalence among people with COVID-19 was generally lower than national prevalence.
-
Current smokers were at reduced risk of testing positive for SARS-CoV-2 compared with never smokers.
-
Former smokers were at increased risk of hospitalisation, disease severity and mortality,
-
while data on COVID-19 outcomes for current smokers were inconclusive.
-
The authors explain that interpretation of results from the reviewed studies is complicated by several factors, including likelihood of being tested and recording of smoking status.
-
-
What is clear is that stopping smoking brings rapid improvements in respiratory and cardiovascular health, benefiting individuals and reducing the risk of acute events requiring hospital admission at a time of intense pressure on the NHS.
-
Public Health England has published COVID-19 advice for smokers and vapers
Physical Health
General and physical health
It is expected that long-term conditions will have worsened for many people over the course of lockdown and there are particular concerns about the impact of delayed cancer diagnoses and the knock-on effects as NHS services are resumed. There is also increasing evidence that people who experience mild to moderate COVID-19 disease may experience a prolonged illness with frequent relapses.
Further evidence
Unequal impact? Coronavirus, disability, and access to services: government response to the
Committee’s fourth report
-
The House of Commons Women and Equalities Committee published the original report in December 2020, and this is the government response.
-
It replies to the recommendations on food accessibility, the Public Sector Equality Duty, and the impacts on health and social care and education among others.
-
It also outlines plans for the National Strategy for Disabled People, to be published in spring 2021.
The multiple conditions guidebook – one year on
-
This Taskforce on Multiple Conditions
report, revisits seven of the case studies featured in the multiple conditions guidebook to find out how things are progressing in the year since their original publication.
-
And in a year that has been extraordinary for everyone, the pandemic has presented some particular challenges for people living with multiple long-term conditions
The impact of the COVID-19 pandemic on cancer deaths due to delays in diagnosis in England, UK: a national, population-based, modelling study
-
Since a national lockdown was introduced across the UK in March, 2020, in response to the COVID-19 pandemic, cancer screening has been suspended, routine diagnostic work deferred, and only urgent symptomatic cases prioritised for diagnostic intervention.
-
In this study, published in the Lancet, the authors estimated the impact of delays in diagnosis on cancer survival outcomes in four major tumour types.
The report suggests that being severely overweight puts people at greater risk of hospitalisation, Intensive Care Unit (ICU) admission and death from COVID-19, with risk growing substantially as body mass index (BMI) increases.
-
The current evidence does not suggest that having excess weight increases people’s chances of contracting COVID-19.
-
However, the data does show that obese people are significantly more likely to become seriously ill and be admitted to intensive care with COVID-19 compared to those with a healthy BMI.
Millions more people with higher health risks due to obesity
-
Each week Nuffield Trust present analysis of data in chart form to illustrate some key issues and invite discussion.
-
To the long list of health problems associated with obesity – from heart disease and type 2 diabetes to osteoarthritis and kidney disease – we can add Covid-19.
-
A number of studies of the risk factors linked to the coronavirus suggest that being overweight is associated with a significantly higher risk of death. (Chart only).
Mental Health
Mental health and wellbeing
Experience from previous pandemics and economic shocks suggests that mental ill health will increase widely during the pandemic, although the scale is difficult to predict. A range of factors may be drivers of poor mental health, including those directly related to COVID-19 (e.g. more generally or because of the loss of family and friends to COVID-19) and those indirectly related through the effects of the social distancing and lockdown measures (e.g. through social isolation or because of financial insecurity).
Suicide
-
Cheshire and Merseyside data up to Week 29 of 2020 (to 24th July), shows that the number of cases so far are similar to that seen in 2019
-
To date there is a lack of clear evidence linking suicides with coronavirus/lockdown (as of end of July 2020) – but this will be monitored closely as more information becomes available
-
See previous Wirral Suicide Audits
Further Evidence
COVID-19 mental health and wellbeing surveillance: report
- This is a routinely updated report about population mental health and wellbeing in England during the COVID-19 pandemic. COVID-19 mental health and wellbeing surveillance: report - GOV.UK (www.gov.uk)
Coronavirus: the consequences for mental health
-
This research from Mind with almost 12,000 people found that those with mental health problems report an increase in the severity of challenges they're facing now and concerns about the future.
-
The authors call for services to be ready for the increase in severity of people's mental health problems, and to take into account the trauma that people have experienced over the past year and how this might affect the support they need.
Out of the woods? Young people's mental health and labour market status as the economy reopens
-
Much has been said about the plight of young people during the Covid-19 crisis, both in terms of their labour market and mental health circumstances.
-
This Resolution Foundation briefing provides an update on how young people were faring at the end of May 2021, shortly after the major relaxation of Covid-19 restrictions in mid-May.
Fit for purpose? Addressing inequities in mental health research exacerbated by Covid-19
-
This Centre for Mental Health report was produced on behalf of the Mental Health Research Group, an independent group of leaders in mental health in England.
-
It highlights the inequities in mental health research funding and production, what gets investigated and who gets to contribute, as well as who and what is left out of the conversation.
-
It shares examples of work taking place to address mental health inequalities and to challenge inequities of power and influence within mental health research.
-
The report calls for systemic change in the ways mental health research is planned, funded, and delivered in the wake of the Covid-19 pandemic
Prevalence, management, and outcomes of SARS-CoV-2 infections in older people and those with dementia in mental health wards in London, UK: a retrospective observational study.
- This research published in The Lancet Psychiatry suggests people living in group situations or
with dementia are more vulnerable to infection with severe acute respiratory syndrome
coronavirus 2 (SARS-CoV-2). - Older people and those with multimorbidity have higher mortality if they become infected than the general population. However, no systematic study exists of
COVID-19-related outcomes in older inpatients in psychiatric units, who comprise people from these high-risk groups. - The authors aimed to describe the period prevalence, demographics,
symptoms (and asymptomatic cases), management, and survival outcomes of COVID-19 in the
older inpatient psychiatric population and people with young-onset dementia in five National
Health Service Trusts in London, UK, from March 1 to April 30, 2020. - Implementation of the longstanding policy of parity of esteem for mental health and planning for future COVID-19 waves in
psychiatric hospitals is urgent.
COVID-19 mental health and wellbeing surveillance: Spotlights (November 2020)
-
Spotlight reports are part of the COVID-19: mental health and wellbeing surveillance report.
-
They describe variation among the population.
Worst hit: dementia during coronavirus ‘Exhausted’ family and friends spent 92 million extra hours caring for loved ones with dementia
since lockdown
-
Since the coronavirus (Covid-19) lockdown on 23 March, this investigation found family and friends have spent an extra 92 million hours caring for loved ones with dementia.
-
This is due to the double impact of lockdown making dementia symptoms worse, and the chronically underfunded social care system leaving them nowhere else to turn.
-
It states that the government must fix social care now, learning lessons to avoid further winter tragedy, as dementia carers struggle with depression, insomnia, and exhaustion.
Coronavirus (COVID-19) Review: data and analysis, March to October 2020
-
A thematic overview of the coronavirus (COVID-19) pandemic between March to October 2020 and
-
how Office for National Statistics data and analysis has been able to provide insight and understanding of the impacts of the pandemic on health, society and the economy.
Mental Health of Children and Young People in England, 2020: wave 1 follow up to the 2017 survey
-
This is the first in a series of follow-up reports by NHS Digital to the Mental Health and Young People Survey (MHCYP) 2017,
-
exploring the mental health of children and young people in July 2020, during the coronavirus (Covid-19) pandemic, and changes since 2017.
-
Experiences of family life, education, and services, and worries and anxieties during the Covid-19 pandemic are also examined.
The impact of Covid-19 to date on older people’s mental and physical health (October 2020)
-
This Age UK research finds that some older people are coping with the pandemic, but a sizeable minority are finding life incredibly tough.
-
Those who are not very well and have long-term health conditions were particularly likely to report that this is an extremely challenging time for them.
-
The research was made up of a survey of older people, their friends, families, and loved ones (promoted across the Age UK social media channels for two weeks in August 2020 and completed by 569 people) and representative online polling of 1,364 people over the age of 60,
conducted by Kantar Polling in September 2020.
Covid-19 and the nation's mental health (October 2020)
-
A new study from the Centre for Mental Health estimates that 8.5 million adults and 1.5 million children in England will need support for depression, anxiety, post-traumatic stress disorders and other mental health difficulties in the coming months and years.
-
This is the equivalent of 20% of all adults and 15% of all children.
-
The report says two-thirds of the people who will need support have existing mental health difficulties and may already be receiving care and treatment.
-
The pandemic may mean they need more support, while others will need help with their mental health for the first time.
Depression in British adults doubles during coronavirus crisis (August 2020)
- The Guardian are reporting that the ONS study shows almost 20% experienced depression, with female, younger and disabled adults most affected
The mental health emergency: how has the coronavirus pandemic impacted our mental health?
-
A survey of more than 16,000 people during lockdown by the charity Mind has revealed the scale of the impact of the pandemic on people with mental health problems.
-
Two out of three (65 per cent) adults over 25 and three-quarters (75 per cent) of young people aged 13-24 with an existing mental health problem reported worse mental health.
The mental health effects of the first two months of lockdown and social distancing during the COVID-19 pandemic in the UK. IFS Working Paper IFS Working Paper W20/16 (Institute of Fiscal Studies (IFS) (June 2020)
-
This report finds that the COVID-19 episode has had substantial negative impacts on mental health across the population.
-
The biggest impacts have been on the gender and age groups – broadly women and the young – that already had relatively low levels of mental health.
-
Pre-existing inequalities in mental health have therefore been exacerbated by the crisis.
COVID-19: guidance on supporting children and young people’s mental health and wellbeing (Public Health England)
-
Advice for parents and carers on looking after the mental health and wellbeing of children or young people during the coronavirus (COVID-19) outbreak. Updated with guidance on 'support bubbles'.
Covid-19 related research and studies
Living online: the long-term impact on wellbeing (UK Parliament, December 2020)
-
Our reliance on digital technology has been greatly accelerated by the Covid-19 pandemic.
-
This inquiry aims to look into the long-term effects this could have on our social and economic wellbeing, focusing on physical health, mental health, social interaction and quality of working life.
Communities at risk: the early impact of COVID-19 on ‘left behind’ neighbourhoods (July 2020)
-
A 'data dive' for the All-Party Parliamentary Group for 'left behind' neighbourhoods. 225 neighbourhoods across England already identified as ‘left behind’ prior to the pandemic are likely to suffer more because of the impact of COVID-19 but have received less emergency funding and support than other areas.
-
The research finds that, although it is early days and results are provisional, COVID-19 is likely to have a long-term negative impact on the most ‘left behind’ neighbourhoods, particularly in relation to employment and health.
UK prevalence of underlying conditions which increase the risk of severe COVID-19 disease: a point prevalence study using electronic health records
-
This study describes the population at risk of severe COVID-19 due to underlying health conditions across the United Kingdom in 2019 using anonymised records.
-
The population were at risk due to a record of at least one underlying health condition, including:
-
8.3% of school-aged children,
-
19.6% of working-aged adults, and
-
66.2% of individuals aged 70 years or more.
-
7.1% of the population had multimorbidity.
-
-
Institute for Fiscal Studies report aims to bring together what has emerged so far about the impacts of the COVID-19 crisis on inequalities across several key domains of life.
-
It argues that the years leading up to the COVID-19 crisis, and in particular the hangover from the last economic crisis of the late 2000s, had already left households in a precarious position.
The geography of the COVID-19 crisis in England
-
This Institute for Fiscal Studies report analyses how the health, economic and social impacts of COVID-19 vary around England.
-
It explores which local authorities (LAs) have residents who are
-
more vulnerable to severe COVID-19 symptoms because of their age or pre-existing conditions;
-
which LAs have a greater share of workers in shut-down sectors such as retail or hospitality; and
-
which LAs have a greater share of children either eligible for free school meals or receiving children’s social services, who might be at particular educational or social risk from the crisis.
-
Characteristics of people testing positive for the coronavirus (COVID-19) in England from the COVID-19 Infection Survey
Main points
-
In this ONS article, they refer to the number of coronavirus (COVID-19) infections within the community population in England; community in this instance refers to private residential households, and it excludes those in hospitals, care homes or other institutional settings.
-
Infections refer to those identified from a positive test for coronavirus (COVID-19) from a swab taken from someone’s nose and throat; this means there was evidence that they had the coronavirus when the swab was taken.
-
Individuals working outside the home show higher rates of positive swab tests than those who work from home.
-
Over the study period, infection rates are higher for those working in patient-facing healthcare or resident-facing social care roles than for people not working in these roles.
-
There is some evidence to suggest that infection rates are lower in one- and two-person households than in larger households.
-
While those who have symptoms are more likely to test positive than those without symptoms, out of those within our study who have ever tested positive for COVID-19, 33% reported any evidence of symptoms around the time of their positive swab test.
-
There is evidence to suggest that infection rates are higher among people who have reported coming into recent contact with a known case of the coronavirus than those who have had no reported contact with potential cases.
-
It is too early to say whether COVID-19 infection rates differ between ethnic groups because the number of people testing positive in groups other than the White ethnic group are very small, although antibody test results provide an indication that individuals identifying as White are less likely to have had COVID-19 in the past than non-white ethnic groups.
REACT-2 study of coronavirus antibodies: June 2020 results
-
Results of real-time assessment of community transmission – prevalence of coronavirus (COVID-19) antibodies in June 2020.
-
The first report from the world’s largest home antibody testing programme tracking who has been infected by COVID-19 in England has today been published.
-
The study tracked the spread of infection across England following the first peak of the pandemic.
-
Findings published by Imperial College London today suggest that 6% of the population in England, around 3.4 million people, have been infected with COVID-19.
-
Key findings of the report on the national home testing study include:
-
In London, 13% of people had antibodies while in the South West of England it was less than 3%.
-
The study showed high rates in those with people-facing jobs in care homes (16%) and health care (12%), compared to 5% of people who were not key workers.
-
There were far higher rates in people from Black (17%), Asian (12%) and other (12%) than white (5%) ethnicity. Work is underway between the Department of Health, local Directors of Public Health and local authorities to understand and mitigate risks of transmission for BAME communities at a local level.
-
Almost everyone with a confirmed case of COVID was found to have antibodies (96%).
-
Those aged 18 to 34 were most likely to have antibodies (8%) with the lowest prevalence in those over 65 (3%).
-
People living in the most deprived areas had higher antibody levels than those in the wealthiest areas (7% compared with 5%).
-
People living in households of more than 6 or 7 people (12%, 13%) were more likely to have had the virus compared to those living alone or with one other (5%)
-
People who smoked were less likely to have antibodies than non-smokers (3% compared to 5%).
-
32% of people reported no symptoms, and this was more common in people over 65 (49%).
-
-
Testing positive for antibodies does not mean you are immune to COVID-19. Currently, there is no firm evidence that the presence of antibodies means someone cannot be re-infected with the virus.
Health and Wellbeing Boards reset tool: support HWB chairs move into the next age of COVID-19
-
Local Government Association (LGA) has developed this tool to support the chairs of Health and Wellbeing Boards (HWBs) in moving into the next stage of COVID-19.
-
It states that the LGA can offer free bespoke support to HWBs during this 'reset phase', ranging from a telephone call to talk through issues and planning a meeting to a virtually facilitated workshop to help reset the HWB.
Levelling down: the medium term local economic impact of coronavirus
-
The Social Market Foundation released analysis on the industries, places and groups face the greatest economic risk over the medium-term period (2020-2023) as a result of coronavirus.
-
The report and their data are available down to local authority level. Overall, their analysis finds:
-
Areas of London face the highest proportion of jobs in moderate or severely impacted sectors (Camden 79%)
-
Areas of the North West tend to fall mid-table in terms of impact
-
As a proportion of jobs in moderate or severely impacted sectors, areas of the Liverpool City Region score as follows: East Merseyside 67%, Liverpool 64%, Sefton 64%, and Wirral 60%
-
Note - highest in research is Camden at 79% and lowest is Anglesey at 54%
- Search SMF report by area
-
Coronavirus (COVID-19): the impact on prisons
-
COVID-19 presents an unprecedented public health crisis that has put additional pressure on a prison system already in a state of crisis.
-
This House of Commons Justice Committee Report looks at the measures the Ministry of Justice and HM Prison and Probation Service have taken in response, focusing primarily on regime changes and strategies to manage the prison population.
Insight from public and across the sectors
The information in this section looks to gather content at both local and national level. We seek to report the growing evidence as to the key issues being faced by people in Wirral and across the UK as they respond and deal with the outcomes of the pandemic. We would welcome research, evaluations or survey results as contributions to add to this local knowledge, email us at wirralintelligenceservice@wirral.gov.uk
How people and communities are coping in the pandemic
Stories from the Pandemic: Age UK Wirral (September 2021)
-
Speculation about a national lockdown intensified during early March, but without any formal government directives, organisations and employers up and down the country were grappling with the conflict between making their own decisions or waiting for formal announcements.
-
This collection of personal reflections identifies the impact the pandemic had on people and how people responded to the needs of their community and those close to them.
Stories of shielding: life in the pandemic for those with health and care needs
-
When lockdown began, Local Voices created a digital platform – Our Covid Voices – for people with health and care needs to share their experiences of the impact of the pandemic.
-
This provided the unfiltered views and stories from people at great risk of all the effects of the pandemic, including anxiety, uncertainty, and changes to their care. Contributors also discuss their relationships, their jobs and dealing with the everyday aspects of life in the pandemic.
-
This National Voices report is a compilation of the contributions, to help inform any decisions taken in the future regarding the way the needs of this group of people are addressed.
Covid-19: what people are telling Healthwatch England about their pandemic experience? (September 2020)
-
This briefing looks at the key issues the public have faced during the Covid-19 pandemic
-
It ranges from the affect lockdown has had on carers, to the problems getting emergency dental treatment.
Wellcome Monitor 2020: Covid-19 study
-
This report presents the results of the fifth Wellcome Monitor.
-
It looks at findings around the British public’s experience of the Covid-19 pandemic and their views on health information during lockdown.
ONS | Unity and division in Great Britain since the onset of the coronavirus (August 2020)
This release from the ONS uses the weekly Opinions and Lifestyles Survey to collect peoples perceptions of unity and division in Great Britain. Some of the key points from this released include:
-
From 24 April to 28 June 2020, more adults on average thought that Britain will be united after we have recovered from the coronavirus (COVID-19) pandemic (46%) than thought that we were united before the pandemic (24%).
-
There was only a small difference in the proportion of the population who thought that Britain would be equal after the pandemic (22%) compared with those who thought it was equal before (19%).
-
Perceptions of how kind people in Britain will be after we recover from the coronavirus pandemic declined from 67% at the start of the period to 56% at the end of the period.
Communities at risk: the early impact of COVID-19 on ‘left behind’ neighbourhoods (July 2020)
-
A 'data dive' for the All-Party Parliamentary Group for 'left behind' neighbourhoods.
-
225 neighbourhoods across England already identified as ‘left behind’ prior to the pandemic are likely to suffer more because of the impact of COVID-19 but have received less emergency funding and support than other areas.
-
The research finds that, although it is early days and results are provisional, COVID-19 is likely to have a long-term negative impact on the most ‘left behind’ neighbourhoods, particularly in relation to employment and health.
Public perceptions of health and social care in light of COVID-19
- Results from an Ipsos MORI survey commissioned by the Health Foundation (May 2020)
- Latest results - July 2020
Financial support for voluntary, community and social enterprise (VCSE) organisations to respond to coronavirus (COVID-19)
- The government has pledged £750 million to ensure VCSE can continue their vital work supporting the country during the coronavirus (COVID-19) outbreak, including £200 million for the Coronavirus Community Support Fund, along with an additional £150 million from dormant bank and building society accounts.
How Community, Voluntary and Faith Sector is coping?
Health charities and the NHS: a vital partnership in peril?
-
This London School of Economics and Political Science (LSE) report was commissioned by range of partners.
-
The report focuses on the work of the charities, in particular their vital performance through the pandemic in hugely challenging circumstances.
-
It highlights the enormous benefits that they could bring to the public’s health and care and calls for a stronger partnership between charities and the NHS so that their contribution can have an even bigger impact in the future.
The impact of COVID-19 on the health and care voluntary sector
-
The health and care voluntary sector continues to provide invaluable information and support to millions of people with long-term conditions as statutory health and care services refocus their efforts on COVID-19.
-
National Voices, together with the Arthritis and Musculoskeletal Alliance (ARMA) and the Neurological Alliance, asked its members about the impact of the coronavirus emergency on their services and their income.
-
Forty charities responded between 17 April and 13 May 2020.
Some consequences of the lockdown changes
Investigation into government funding to charities during the Covid-19 pandemic (May 2021)
-
In 2020, the government announced a £750 million financial support package for frontline charities.
-
It designed the package as part of its response to the Covid-19 pandemic.
-
It targeted its support at those organisations in the voluntary, community and social enterprise sector providing vital services to the vulnerable.
-
This National Audit Office report explores the Department for Digital, Culture, Media and Sport’s distribution and oversight of £513 million of the package.
-
It considers how the Department allocated funds, how financial support could be accessed by the sector and where financial support was received.
Councils spending thousands on 'littering epidemic' in parks
- Councils have been forced to spend an extra £33,000 on average dealing with litter and anti-social behaviour in parks since lockdown was eased, according to a new survey.
Below: Graphic of the Immediate mental health impact of COVID-19 across life course
The Local Government Association (LGA) and the Association of Directors of Public Health (ADPH) have jointly produced this briefing about the public mental health and wellbeing issues arising from the COVID-19 outbreak.
While many people have acted in solidarity in response to COVID-19, and there will be some positive benefits from this community spirit and response, the epidemic will likely have many psychological impacts on the population which may have a detrimental effect on the short, medium and long-term mental health of some residents.